Why diabetic foot ulcers aren’t healing, and what to do about it

Diabetes is one of the most common diseases amongst adults in the UK, affecting roughly 4.3 million people and responsible for 174 amputations every week. Diabetic foot ulcers occur in between 10% and15% of people living with diabetes and, if left unmanaged, can lead to serious complications for the individual.
What causes diabetic foot ulcers?
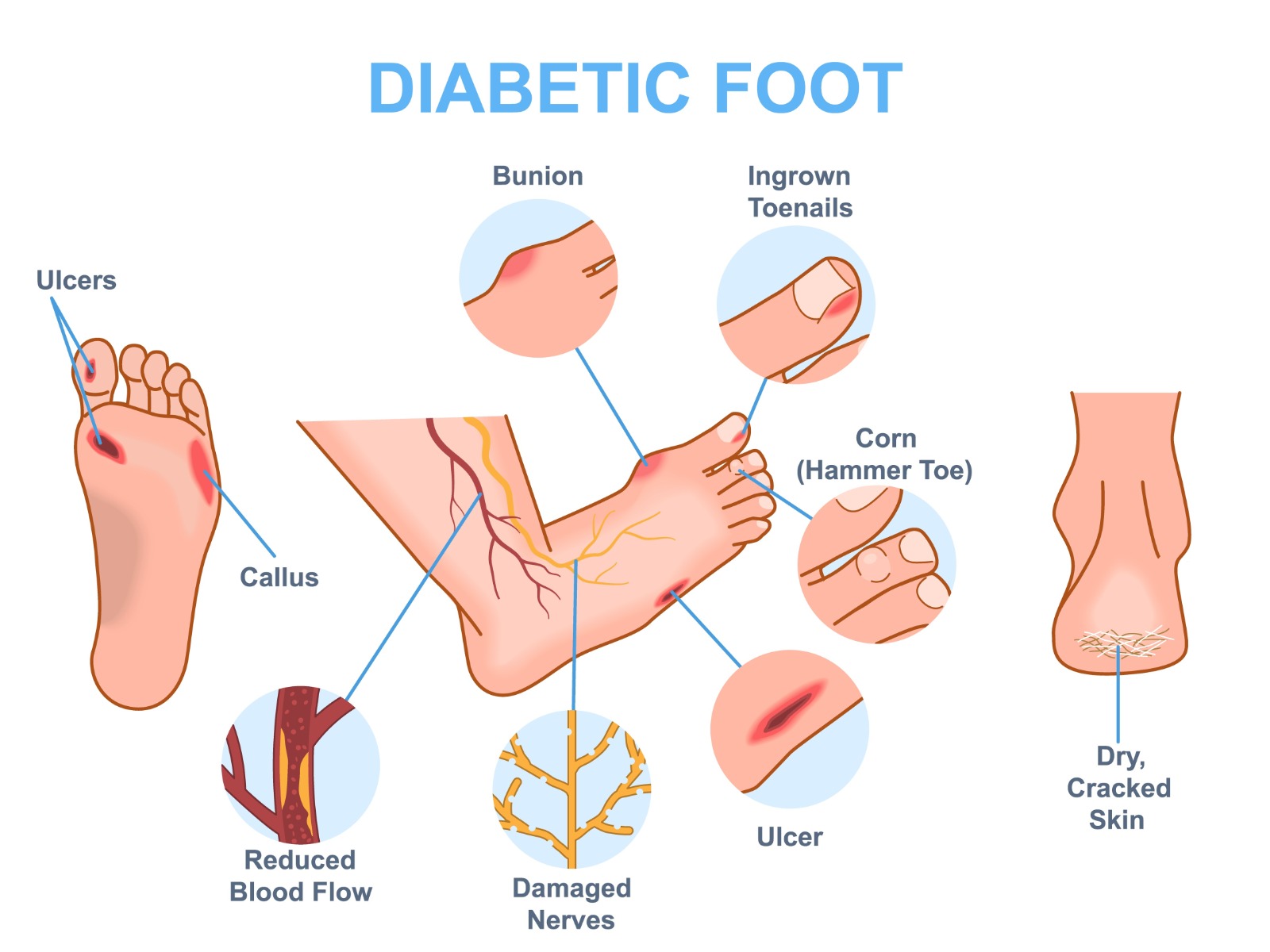
Diabetes affects people in a myriad of ways, especially when not controlled. High blood sugar as a result of poorly managed diabetes can do long-term damage to the macrovascular and microvascular blood vessels and nerves, resulting in poor circulation and/or reduced sensation in the outer extremities.
To understand how this affects someone with diabetes, you need to be aware of the different types of neuropathies, or nerve damage, that diabetes causes:
- Motor neuropathy: decreased motor nerve conduction means that the electrical impulses that move through the nerves is slower or compromised compared to that of someone without the condition
- Sensory neuropathy: often a direct complication of another comorbidity, this is damage to the nerves that carry messages of touch, temperature, pain etc.
- Autonomic neuropathy: damage to the nerves that control automatic body functions, including blood pressure and temperate control
When a callus, irritation, or trauma develops on the foot, usually caused by motor neuropathy, there is a higher risk of it going unnoticed due to the effects of sensory neuropathy. Drying of the skin, which is caused by autonomic neuropathy, means that over time, prolonged trauma to the area can turn into an open wound.
Why do diabetic foot ulcers take longer to heal than other types of wounds?
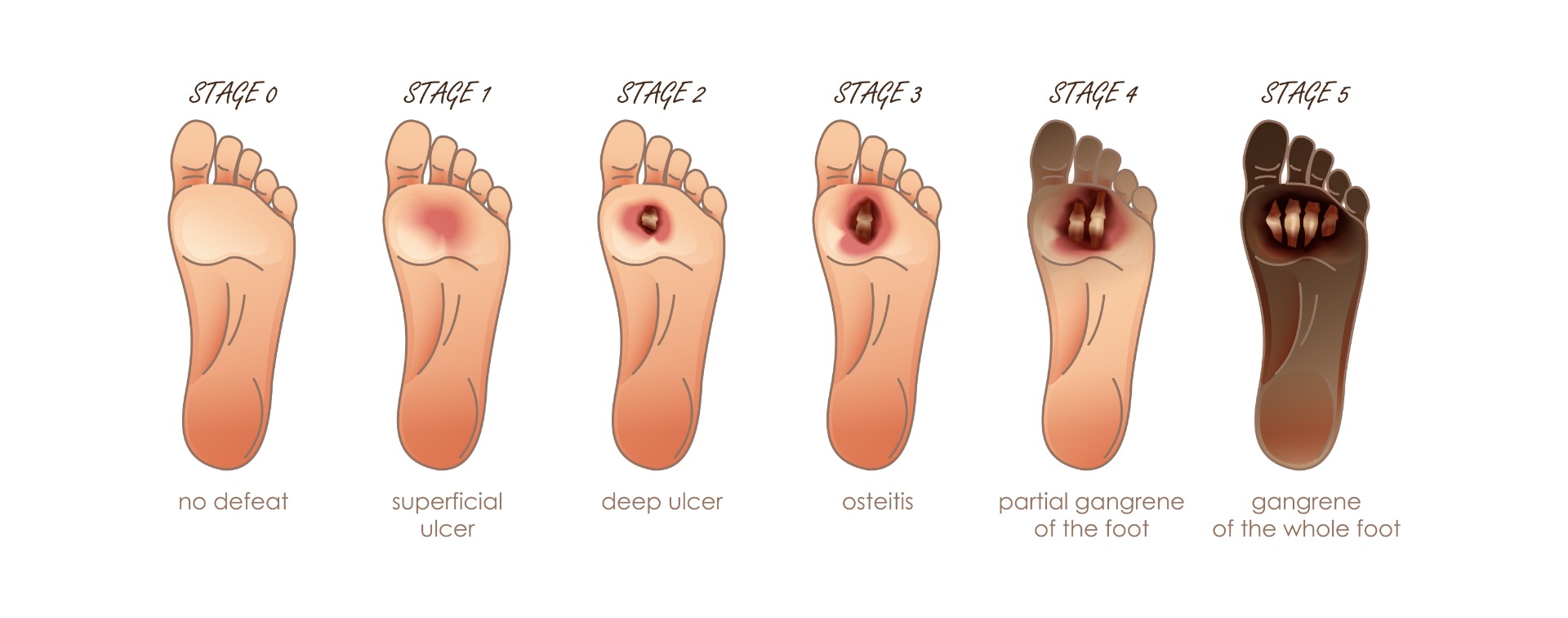
As much as vascular issues exacerbate the causes of foot ulcers, they can also lead to prolonged healing times, complications, and even amputation. Often with diabetic foot ulcers, because blood is unable to effectively reach the area to help bolster the healing process, there is a heightened chance of infection, necrosis, and gangrene.
What is the best course of action for diabetic foot ulcers?
Diabetic foot ulcers can become very serious very quickly, so it is crucial that they are taken care of as soon as possible in order to reduce the risk of infection, amputation, and to improve function of the lower limb. The best way to mitigate this is through prevention. Pressure off-loading devices such as the Levabo Heel-Up are designed to prevent, manage, and treat diabetic foot ulcers by reducing the pressure and friction put on the foot. It is also recommended to use an intense moisturising and anti-microbial cream on the feet to stop skin dryness that can lead to calluses or cracks.
If an ulcer is already present, removing the dead skin and tissue (debridement) can help to stop further necrosis and infection. As with any other wound, ensuring the area is clean, dressed, and – if necessary – medicated, alongside the use of a pressure offloading device, will help to ensure healing of the area.
Healing time depends on the size, location, and pressure on the wound, as well as blood glucose levels and general wound care. If you or a loved one is at risk of diabetic foot ulcers, it is important to contact a podiatrist or tissue viability specialist to ensure a robust prevention and care plan is in place.
At Algeos, we work with leading brands in diabetes and pressure care to provide what you need to properly look after your feet, and ultimately keep you moving.
To view our range of diabetic and pressure care products, visit: https://www.algeos.com/pressure-care-and-diabetes







